

The Expert: Dr. Peter H’Doubler, a vascular surgeon in Atlanta, testified for the defense, detailing the procedure and his belief that the defendant doctor met the standard of care in treating the patient.
Testifying in a 2015 medical malpractice trial, Dr. Peter H’Doubler, a vascular specialist affiliated with Emory University, speaks to the standard of care for the placement of a dialysis catheter by way of the internal jugular vein. The case involved the plaintiff’s claim that the surgeon placing the catheter breached the standard of care when the heart was perforated during the procedure, which caused the patient’s death.
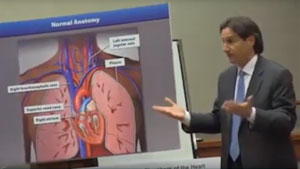
H’Doubler uses multiple visual props to get his points across for the defense. He begins by describing the placement of a guiding wire through the needle used to access the vein in the neck. The needle can then be removed and the wire carefully guided through the vein pathways into either the superior or inferior vena cava, just as they enter the heart. This wire is then used as a “rail” to pass the dialysis catheter over, and theoretically the wire is then removed and the catheter is left in place where maximum blood can be accessed for dialysis without causing difficulties with the heart or blood vessel side walls.
In this case, however, the patient had had several previous catheterizations, which had caused significant scarring. She had a somewhat anomalous venous pathway, as well. These two factors caused difficulty in feeding the wire into the proper location, so the surgeon had opted to use a much thicker wire to gain access. The plaintiffs felt that the use of this wire was questionable and resulted in the injury to the heart that killed the woman.
However, the expert disagreed with this contention, and says that not only was it indicated to use the stiffer wire, but it should be safer, demonstrating that the last four centimeters of the wire are very floppy. Drawing upon his vast experience in dealing with this type of problem, he notes other colleagues that have gotten into trouble by not using the stiffer wire with the floppy advancing end when faced with anomalous, scarred veins.
The defense had previously testified that the surgeon monitored, by fluoroscopy, the advancement of the catheter over the wire and its difficulties in maneuvering through the tortuous veins when the distal part of the wire perforated the heart muscle. The plaintiff offered that the surgeon should have been focused on the wire tip instead since it was in danger of doing exactly what had happened. H’Doubler disagreed with the plaintiff’s contention and states that the surgeon had done exactly what he himself would have done when having difficulty passing the catheter over the guiding wire. There is just as much threat to the tortuous and scarred veins where the catheter is trying to get through, H’Doubler tells the jury, as there is at the floppy end of the wire. He adds that he would have expected that the wire would remain in place while performing the maneuvers with the catheter.
Taking into account the timing of events as they occurred, the expert states that the perforation occurred when the coiled energy within the guiding wire was released as the difficult catheterization was withdrawn. The coiled wire, he explains, could theoretically have sprung forward and pierced the heart wall. This would have created a very tiny hole that perhaps allowed 1cc of blood to escape the heart with each beat, into the intact pericardial sac around the heart. At first, this would not be a problem, but assuming the patient’s heart beat 60 times a minute, that would be 60 cc of blood collecting in the closed sac of the pericardium each minute. After five minutes there would be 300 cc of blood trapped under pressure in the pericardium, which is more than enough to prevent the heart from filling and emptying properly. This condition is known as pericardial tamponade and is life threatening.
The expert’s testimony helped yield a defense verdict in the case.
Gary Gansar, MD, is residency-trained in general surgery. He served as Chief of Surgery and Staff at Elmwood Medical Center and on the Medical Executive Committee at Touro Infirmary and Mercy Hospital in New Orleans, LA. Dr. Gansar was Board Certified in general surgery while in active practice. He joined AMFS in 2015 as a Physician Medical Director.
The medical expert witness partner for attorneys serious about building a winning case
AMFS is your trusted source for highly-qualified medical expert witnesses. After pioneering the field nearly three decades ago, we’re continuing to redefine medical expert witness services by providing value far beyond a referral alone.
Our Physician Medical Directors know what it takes to build a strong case. Our medical expert witnesses leave no doubt. And our case managers streamline billing and logistics every step of the way, letting you focus on what you do best: constructing your winning case. Explore why AMFS clients expect more from their medical expert witnesses—and get it.
