

The Expert: Dr. Gordon Sze, a professor of radiology and biomedical imaging at Yale, details the patient’s condition as well as the difference between different brain bleed episodes, concluding the patient’s outcome was not caused by unchecked hypertension.
While giving testimony in a 2015 Florida medical malpractice trial, Dr. Gordon Sze, a professor of radiology and biomedical imaging at Yale, is asked to comment on whether physicians might have saved the life of a woman who died of stroke complications had they taken action to lower her blood pressure.
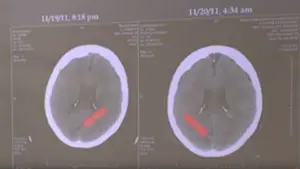
To substantiate his opinion regarding this question, the doctor first explains the difference between a hypertensive bleeding episode and hemorrhagic transformation of an ischemic stroke. In doing so, he contrasts the pathophysiology, anatomical propensities, and the appearance on CAT scan images of these two types of brain hemorrhage to support his opinion that the plaintiff’s wife suffered a hemorrhagic transformation of a cerebral embolism that would not have been prevented by lowering her blood pressure.
Serial CAT scans of the patient’s brain documented ischemic events occurring 12 hours earlier than the initial films, followed by reperfusion injury in those areas of the brain about 8 hours later. The ischemic events were most likely caused by embolisms (arterial plaques that ruptured and travelled to parts of the brain, blocking blood flow to it) that occurred around the same time within different areas of the brain fed by the basilar artery. This phenomenon, of multiple simultaneous ischemic events in different areas of the brain fed by the same arterial system, is not unusual and is seen on the studies as dark areas of dead tissue. Hours later, these damaged sites begin to slowly bleed as the blood is no longer contained within the infarcted structures. This is seen on the CAT scan as faded white areas within the dark infarctions.
An active arterial bleed that is not preceded by ischemic damage, but is instead related to a blood vessel rupturing under pressure, will appear immediately as a very bright white spot on the CAT scan. That is because the large amount of escaped blood is pushing aside the normal brain tissue as a mass effect. This shows up as a homogenous, bright white mass. The blood from hemorrhagic transformation on the other hand, appears as “cream poured over chocolate cake.” This slow ooze of blood through damaged brain tissue dilutes the white appearance making it less prominent.
The mass effect, sometimes seen in hypertensive hemorrhagic strokes, can lead to disruption of the drainage of the brain ventricles and cause those ventricles to dilate. This phenomenon is not generally seen with lower pressures of hemorrhagic transformation, Sze tells jurors, as he points out that ventricular dilatation is not seen in this case.
Sze demonstrates how the earlier films show the dark shadows caused by damage from embolic ischemia, and there is no white representing blood on these sections. Eight hours later, the faded white appearance of blood is noted, as the damaged areas begin to slowly leak blood into them. This is hemorrhagic transformation and occurs regardless of the patient’s blood pressure.
Using CAT scans that represent classic examples of hypertensive hemorrhage, rather than the patient’s films, Sze easily demonstrates that the phenomena of hypertensive hemorrhage and hemorrhagic transformation look nothing alike on these type of studies, nor do they tend to occur in the same anatomical areas of the brain. The former injury rarely appears in the cerebellum as the injuries to the patient did.
Posterior reversible encephalopathy syndrome, or PRES, is another syndrome related to high blood pressure within the brain. It presents as fluid leaking out of the blood vessels more diffusely, symmetrically, and bilaterally, which is not what was seen in this case. Lacking any radiologic evidence supporting the plaintiff’s claim, the professor concludes that there was no hypertensive event in this case. He agrees that embolic plaques led to ischemic infarctions that were probably 12 hours old when she presented. The patient’s films were consistent with hemorrhagic transformation occurring while hospitalized and which followed the damage caused by the ischemia, rather than hypertensive blood pressure. Lowering the patient’s blood pressure therefore would have not affected the outcome in this case.
The jury agreed with the expert’s persuasive, detailed explanation, giving a judgment for the defense.
Gary Gansar, MD, is residency-trained in general surgery. He served as Chief of Surgery and Staff at Elmwood Medical Center and on the Medical Executive Committee at Touro Infirmary and Mercy Hospital in New Orleans, LA. Dr. Gansar was Board Certified in general surgery while in active practice. He joined AMFS in 2015 as a Physician Medical Director.
The medical expert witness partner for attorneys serious about building a winning case
AMFS is your trusted source for highly-qualified medical expert witnesses. After pioneering the field nearly three decades ago, we’re continuing to redefine medical expert witness services by providing value far beyond a referral alone.
Our Physician Medical Directors know what it takes to build a strong case. Our medical expert witnesses leave no doubt. And our case managers streamline billing and logistics every step of the way, letting you focus on what you do best: constructing your winning case. Explore why AMFS clients expect more from their medical expert witnesses—and get it.
