

The Expert: Dr. Matthew Lotysch, a California radiologist testifying for the defense, who concludes there is no evidence of a hypoxic injury to the child’s brain that would have been caused by drowning.
In a 2021 negligence trial from the Orange County Superior Court of California, Dr. Matthew Lotysch, a diagnostic radiologist from Los Angeles, offers expert testimony for the defense. The case, Hudson v. Northwest Hotel Corp., involved a near drowning of a six-year-old girl in a hotel hot tub. The trial testimony in this video clip addresses whether there was an actual traumatic brain injury from hypoxia due to drowning, or as the defense contends, that the child suffered brain damage due to a viral infection that was totally unrelated to the hot tub incident.
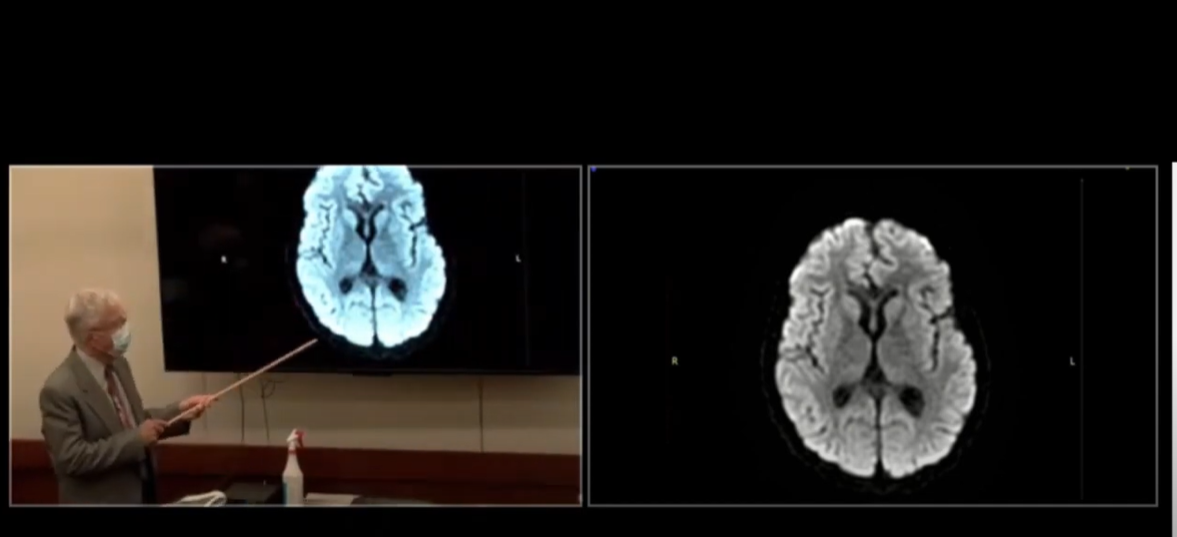
Lotysch uses projections of the child’s MRI’s as well as a hand-drawn MRI replica to elucidate his points. The original MRI was performed on August 20, 2015. This was used as a baseline for comparison of the second MRI done on September 2, 2015. In this video we see only one of about a thousand cross-sectional images taken as a coronal section, or a single slice of the brain at about the level of the nose from the front of the skull to the back. The doctor, having reviewed all of the MRI sequences, states unequivocally that the study was normal and that he is using this one slide as a representative of all that he reviewed to demonstrate that fact. Under questioning, he specifically confirms that there is no evidence of any hypoxic injury or hyperthermal injury on this study.
The expert then discusses the second MRI and he begins by offering that there had to be a change in the patient’s status for a second study to have been ordered. Given that the first study showed no significant pathology, there must have been a change in her condition to order a follow-up study. He then reads from the written history from the physician treating the patient to the radiologist that examined the study: “Previous images and labs normal, but acutely more encephalopathic. MRI to rule out encephalitis vs paraneoplastic.” So the treating physicians were at no point finding evidence of anoxic injury or hyperthermic brain injury from near drowning. Instead, the little girl’s clinical course suggested other things entirely. More specifically, they were searching for signs of infection of the brain or evidence of the body’s antibody response to a tumor of the central nervous system.
The treating physician also anticipated the need for a diagnostic lumbar puncture on the child, asking that this be accomplished during the sedation needed to perform the MRI. Again, this would not be needed if anoxic brain injury were suspected.
The radiologist reading the second MRI ultimately saw no evidence of brain injury related to hyperthermia or hypoxia even with the administration of contrast dye to expose this possibility. Dr. Lotysch explains that the brain requires glucose and oxygen which are carried by the bloodstream. If the blood supply is interrupted, or the oxygen or glucose levels are too low, the brain will become dysfunctional. The MRI images in any patient with hypoxia or ischemia (lack of or low oxygen levels) or hyperthermic injury (high internal body temperature) would be noted as a distinctive pattern of enhancement in particular areas of the brain by the contrast dye that is administered. The doctor sketches these areas out on a poster. These areas that one would expect to see affected would be areas of the brain that require the most oxygen and glucose, the cortical gray matter and the basal ganglia. Once sustaining injury in this way, these areas would die if not soon supplied with the oxygen and glucose that they need.
This crystal-clear explanation was undoubtedly useful to the jury, which declined to award damages in the case.
Gary Gansar, MD, is residency-trained in general surgery. He served as Chief of Surgery and Staff at Elmwood Medical Center and on the Medical Executive Committee at Touro Infirmary and Mercy Hospital in New Orleans, LA. Dr. Gansar was Board Certified in general surgery while in active practice. He joined AMFS in 2015 as a Physician Medical Director.
The medical expert witness partner for attorneys serious about building a winning case
AMFS is your trusted source for highly-qualified medical expert witnesses. After pioneering the field nearly three decades ago, we’re continuing to redefine medical expert witness services by providing value far beyond a referral alone.
Our Physician Medical Directors know what it takes to build a strong case. Our medical expert witnesses leave no doubt. And our case managers streamline billing and logistics every step of the way, letting you focus on what you do best: constructing your winning case. Explore why AMFS clients expect more from their medical expert witnesses—and get it.
