

The Expert: Dr. Harris Fisk, a neurologist, testifying for the plaintiff on the traumatic brain injury, post-traumatic stress disorder, and other complications one of the brothers suffered as a result of the crash.
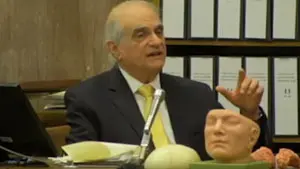
The testimony given by Dr. Harris Fisk during this California trial on damages was crucial to the nearly $53 million verdict delivered to two brothers who were injured in a big rig trucking accident. Fisk calmly takes the jury through discussions of traumatic brain injury, post-traumatic stress disorder, sleep disorder, stress-anxiety-depression disorder, and their possible interactions. These pathologies from different medical fields are informatively brought together by the presentation from this distinctive, experienced neurologist testifying about cutting-edge issues.
Matthew and Michael Lennig were injured in a head-on collision with a semi-truck helmed by a CRST driver. The trucking firm admitted the driver’s negligence but disputed the severity of the brothers’ claimed brain, arm, and back injuries, leading to a trial on the issue of damages alone.
Fisk, a Los Angeles-based neurologist with more than 40 years of medical experience, is called to detail the lasting impact of the crash on Matthew Lennig. The doctor speaks of Lennig’s brain concussion as part of the spectrum of traumatic brain injury causing a variety of symptoms that the victim is now forced to deal with: thinking and memory problems, buzzing in the ears or loss of hearing, behavioral changes, headaches, and dizziness. Fisk also addresses the occipital neuralgia—headaches generated by the actual damage to nerves coming from the base of the skull. This post-traumatic headache syndrome he relates to the actual crushing of the occipital nerves between bones.
Convincingly, the neurologist details what the trauma has physically done to the plaintiff. Post-traumatic vertiginous disequilibrium has taken his balance, benign positional paraxysmal vertigo keeps him dizzy, he is plagued by chronic neck pain from cervical strain, numbness and tingling in the arm, carpal tunnel syndrome affecting his wrist, damage to the chest wall and lower back structures.
Fisk then launches into a discussion of how post-traumatic stress disorder and traumatic brain injury can overlap. The headaches and dizziness, the cognitive problems—thinking and memory, are “physically based disorders” that interact with emotional disorders such as panic, anxiety, and depression in an augmenting spiral. Drawing from both neurologic and psychiatric knowledge, Fisk elaborates on the mechanisms at play, ultimately concluding that the interplay of pathologies here will forever interfere with the victim’s ability to perform as the police officer that he was, while his present ability to work at a desk job does not imply that he is well, nor will he ever be.
The question arises—are these problems actually traumatic brain injury or post-traumatic stress disorder? Does it matter? The neurologist explains that even if the brain injury was to heal, the physical damage to the anatomic structures will prolong the patient’s symptoms. The pain is causing cognitive inefficiency. The victim hurts so much that he cannot think straight, even if his brain has healed.
His final statements here were crucial to sealing the jury’s sympathies. The brain has two years to heal with traumatic brain injury; but we are beyond that. We should know if treatment of post-traumatic stress disorder has been successful within 6 months; but we are beyond that. There is normally a small chance of complete resolution of a patient’s sleep disorders, stress anxiety, depression, and panic disorder with intense treatment if they exist as a singular pathology, but the interaction of all of these pathologies in this one patient “will not be resolved for the remainder of his life.”
Gary Gansar, MD, is residency-trained in general surgery. He served as Chief of Surgery and Staff at Elmwood Medical Center and on the Medical Executive Committee at Touro Infirmary and Mercy Hospital in New Orleans, LA. Dr. Gansar was Board Certified in general surgery while in active practice. He joined AMFS in 2015 as a Physician Medical Director.
The medical expert witness partner for attorneys serious about building a winning case
AMFS is your trusted source for highly-qualified medical expert witnesses. After pioneering the field nearly three decades ago, we’re continuing to redefine medical expert witness services by providing value far beyond a referral alone.
Our Physician Medical Directors know what it takes to build a strong case. Our medical expert witnesses leave no doubt. And our case managers streamline billing and logistics every step of the way, letting you focus on what you do best: constructing your winning case. Explore why AMFS clients expect more from their medical expert witnesses—and get it.
